
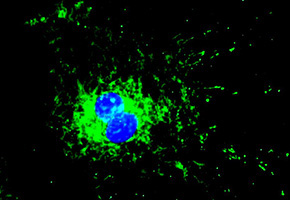
Heart affected by heart failure. The white area indicates the site affected by the induced infarction (photos: ICB/USP. Cover: cardiac cells with nucleus in blue and mitochondria in green)
In preclinical tests on rats, a drug discovered by researchers from the University of São Paulo and Stanford University increases heart function by 40%. Clinical tests are expected to begin in 2014.
In preclinical tests on rats, a drug discovered by researchers from the University of São Paulo and Stanford University increases heart function by 40%. Clinical tests are expected to begin in 2014.
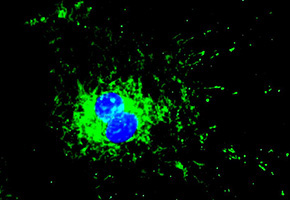
Heart affected by heart failure. The white area indicates the site affected by the induced infarction (photos: ICB/USP. Cover: cardiac cells with nucleus in blue and mitochondria in green)
By Karina Toledo
Agência FAPESP – In preclinical tests, a synthetic molecule developed by researchers at Stanford University in the United States and at the University of São Paulo (USP) has shown the potential to become an ally in the treatment of heart failure and other diseases. Initial tests on humans to determine the compound’s safety are expected to begin in the second half of the year with private funding support.
Known as Alda-1, the drug can activate an enzyme called ALDH2 (aldehyde dehydrogenase-2), which is found in mitochondria and is considered to be critical for the proper functioning of all cells, including cardiac cells.
“This enzyme is of major importance to cells because it helps prevent the accumulation of aldehydes – toxic and highly reactive molecules produced by cells. ALDH2 deficiency has increasingly been associated with various types of diseases,” said Julio Cesar Batista Ferreira, professor in the Department of Anatomy at the Institute of Biomedical Sciences at USP and coordinator of the FAPESP-funded study in Brazil.
In a recent experiment conducted during the master’s degree work of Kátia Maria Sampaio Gomes, a FAPESP scholarship recipient and an advisee of Ferreira, the group treated rats that had cardiac insufficiency with Alda-1 for six weeks and observed a 40% increase in the ability of the rats’ hearts to pump blood.
The findings were published in the June issue of the journal Cardiovascular Research. The project won the “Proof of Concept” category in the 2013 USP Innovation Olympics.
The animal model used in the study simulates one of the principal etiologies of heart failure: acute myocardial infarction. To induce this condition in rats, scientists tie off one of the coronary arteries. The absence of blood supply causes immediate death to approximately 30% of the cardiac cells. The remaining cells begin to work twice as hard to compensate for the injury and ultimately collapse. After one month, the animal already presents signs of heart failure.
“We began treatment with Alda-1 four weeks after the induced infarction, when the animals were already presenting with weakened heart function. After six weeks of treatment, we observed a 40% increase in the volume of blood pumped among the group that received the drug. Heart function had diminished further in the placebo group,” explained Ferreira.
Initial findings
Alda-1 was discovered while Ferreira did post-doctoral work at Stanford, with support from FAPESP.
In a study published in 2011 in the journal Science Translational Medicine, the group demonstrated that by activating the ALDH2 enzyme in cardiac cells, Alda-1 was able to protect the heart after an infarction.
“Today, we know that an excess of aldehydes directly harms mitochondrial metabolism, resulting in lower production of ATP [adenosine triphosphate, the molecule that stores energy] and the release of more reactive molecules, such as free radicals and even aldehydes. When metabolism is compromised, cells end up dying. To this end, Alda-1 plays an important role in that it protects cells from metabolic collapse induced by an excess of aldehydes,” Ferreira explained.
ALDH2’s mission is to eliminate aldehydes, but its activity is often diminished in cardiac cells after infarction or in patients with heart failure. “The excess aldehydes can themselves end up inactivating ALDH2, and it [the enzyme] becomes unable to remove them as efficiently, thus creating a vicious cycle that results in cell death,” Ferreira explained.
In the 2011 article, the scientists showed that one of the drugs most often used in patients with infarction to promote vasodilation – nitroglycerin – further inhibits the activity of ALDH2, accelerating the process of cardiac cell death. However, experiments in rats indicated that the harmful effects of nitroglycerin could be neutralized if Alda-1 is administered simultaneously (read more at: http://agencia.fapesp.br/en/14974).
In a recently published review in the journal Physiological Reviews, the groups from Stanford and USP present an extensive discussion of the role of ALDH2 and the potential treatment opportunities for substances capable of activating the expression of this enzyme.
“Because the aldehydes are able to enter the bloodstream and bind to proteins from distant organs, our hypothesis is that treatment with Alda-1 could prevent the ripple effect that normally occurs in patients with heart failure and that affects other organs,” Ferreira said.
In comparing blood samples from healthy individuals and patients with heart failure, Ferreira’s group observed three times as many circulating aldehydes in the latter group. “We estimate that the level in the heart is 10 times higher,” the researcher said.
Clinical tests
Under the coordination of Daria Mochly-Rosen, a professor in the Department of Chemical and Systems Biology of Stanford, the US group established the startup company Aldea Pharmaceuticals in an attempt to make Alda-1 – still an experimental drug – into a commercial product.
“They ended up obtaining private financing to begin Phase 1 clinical testing, which is basically designed to assess the toxicity of the molecule in healthy individuals. If the tests are successful, they may be authorized to conduct tests on carriers of a particular disease,” Ferreira explained.
Initially, however, the focus of Aldea – which involves no Brazilians – will not be patients with heart failure; instead, the company will focus on carriers of a mutation in the ALDH2 gene that affects 600,000,000 people worldwide (45% of the Asian population, the world’s most common mutation) and that makes them susceptible to the harmful effects of alcohol – a substance that when metabolized releases large amounts of aldehydes.
“This mutation reduces ALDH2 activity up to 95%. People with this mutation are at an increased risk of developing diseases associated with alcohol, such as stomach cancer. And even if they don’t drink, they face an increased risk of suffering from cardiovascular and neuronal diseases because of their difficulty getting rid of aldehydes.” Alda-1 is able to increase the activity of the mutant ALDH2 ten times over, presenting a huge therapeutic potential for individuals with the mutation,” Ferreira explained.
Aldea is also expected to test the effectiveness of the Alda-1 molecule at preventing problems that arise from excessive alcohol consumption and in the emergency treatment of patients with alcoholic coma. According to Ferreira, cardiac disease is another line in which the startup company plans to invest in the future.
“The Stanford researchers are conducting a series of studies to optimize the molecule by modifying its structure to make it more soluble and less toxic and to have a more prolonged effect. We have a contract to test these variants in models in our laboratory,” Ferreira said.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





