

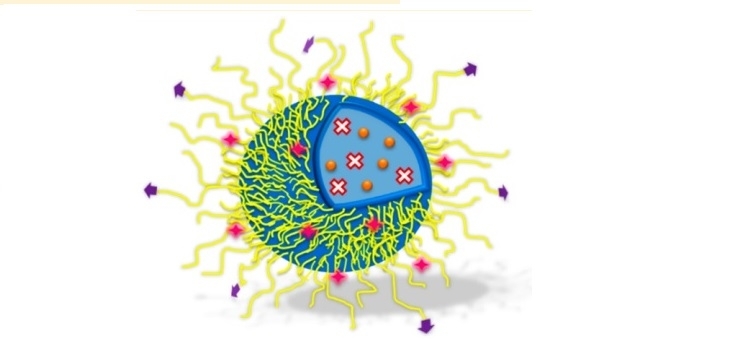
Therapy used against grade four glioblastoma multiforme combines a photoactive molecule and a chemotherapeutic agent – both encapsulated in protein-lipid nanoparticles; work was presented by Antônio Claudio Tedesco during FAPESP Week France (imagem: Molecular Pharmaceutics)
Therapy used against grade four glioblastoma multiforme combines a photoactive molecule and a chemotherapeutic agent – both encapsulated in protein-lipid nanoparticles; work was presented by Antônio Claudio Tedesco during FAPESP Week France.
Therapy used against grade four glioblastoma multiforme combines a photoactive molecule and a chemotherapeutic agent – both encapsulated in protein-lipid nanoparticles; work was presented by Antônio Claudio Tedesco during FAPESP Week France.
Therapy used against grade four glioblastoma multiforme combines a photoactive molecule and a chemotherapeutic agent – both encapsulated in protein-lipid nanoparticles; work was presented by Antônio Claudio Tedesco during FAPESP Week France (imagem: Molecular Pharmaceutics)
By Maria Fernanda Ziegler, from Paris | Agência FAPESP – Researchers from the University of São Paulo (USP) in Brazil have developed a strategy for treating the most aggressive type of brain cancer in adults that combines a photoactive molecule and a chemotherapeutic agent – both encapsulated in protein-lipid nanoparticles
Results of the research, supported by FAPESP, were presented on November 26th, during the FAPESP Week France symposium, by Antônio Claudio Tedesco, of the Center for Nanotechnology, Tissue Engineering, and Photo processes of the Chemistry Department of the Ribeirão Preto School of Philosophy, Sciences, and Arts (FFCLRP-USP).
Grade four glioblastoma multiforme represents almost 25% of all non-metastatic brain tumors. The new therapy can be used before, during, and after tumor removal surgery, which is obligatory in more aggressive cases of glioblastoma. The use of protein-lipid nanoparticles allows for the release of active compounds directly into the tumor in a gradual and sustained way over a number of months.
“The less brain tissue that is removed, the safer the surgery is, since the risk of compromising the patient’s vital functions falls considerably,” explained Tedesco.
Data from experiments carried out on tumorous cell cultures were published in the journal Molecular Pharmaceutics.
The group intends to soon evaluate the effect of the treatment on animals before, during, and after surgical removal of the tumor. The proposal is to enrich the affected region with the photoactive molecules around two weeks before the surgery. During that period, simultaneously, the chemotherapy will be acting to reduce the tumor mass.
During the surgery, the light is applied to activate the photosensitive compounds. “At that moment, with the removal of the skullcap and the tumor, it’s possible to protect the healthy tissue with the phototherapy and kill the diseased cells that may continue impregnated in the tissue,” said the researcher.
In the post-surgical period, the new treatment can help avoid relapse, since the nanoparticles are able to release in a sustained and gradual way the chemotherapy directly into the tumor region, without causing collateral problems in the debilitated patient.
“It’s precisely in that period that 90% of patients present a relapse and, usually, in a very aggressive way. However, as they’re debilitated, it isn’t possible to subject them to radiotherapy or conventional chemotherapy. With the new method, we can maintain an active fight against the disease for a month after surgery,” said Tedesco.
The conventional chemotherapeutic treatment against glioblastoma involves administering the drug temozolomide, at a high cost and with little guarantee of effectiveness. Adverse effects of the dose needed to cross the blood-brain barrier, which protects the central nervous system, include damage to bone marrow, where the hematopoietic stem cells that are responsible for generating blood cells and the immune system are located.
A thousand and one uses
Tedesco highlights that nanotechnology and the new drug delivery systems have enabled molecules that before were used for treating certain pathologies to be “redesigned” and adapted to new functions.
Thus, the same system used for the treatment of glioblastoma can also act in diagnosis and provide important information for the tumor removal surgery by means of a fluorescent marker.
Currently, before surgery, CT or MRI scans capable of detecting the tumor mass are used. “The neurologist decides the margin of safety that should be removed. With the new system, it’s possible to know exactly what mass is to be removed,” he said.
The same carrier systems containing the active compounds described above can also be used for marking and diagnosing less serious types of glioblastoma. “We’d like to use the same approach to identify patients with grade two and three tumors that haven’t yet reached the point of needing surgical intervention. It’s important for us to be able to treat the disease before it evolves,” said Tedesco.
“If we have to go on to surgery, our idea is that, with 3D organ printing technology, already available at the Center for Nanotechnology, we can build a prosthesis with the exact size of the tumor to be removed. We can impregnate this material with chemotherapy, so that it acts in the same way as described above, that is, it presents a sustained release of the active compound over weeks or months,” he said.
Tedesco’s group is one of the pioneers in Brazil in the area dynamic phototherapy. The work in this field began with the treatment of skin cancer and quickly moved on to the area of tissue engineering and organ and tissue regenerative medicine. The studies already carried out include an artificial human skin model – currently produced for treating burns and scarring.
There are also studies with highly specific drug delivery systems that can be used in treating neurodegenerative diseases, such as Parkinson’s, Alzheimer, and epilepsy.
The FAPESP Week France symposium took place between November 21st and 27th, thanks to a partnership between FAPESP and the universities of Lyon and Paris, both in France. Read other news about the event at http://www.fapesp.br/week2019/france/.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





