

DNA vaccines are cheaper and potentially more efficient than inactivated or attenuated virus vaccines (scientist Francine Teixeira performing research at FM-USP; photo: Camilla Adan)
The vaccine is being developed by researchers in Brazil. The results of preclinical trials are published in the journal Frontiers in Immunology.
The vaccine is being developed by researchers in Brazil. The results of preclinical trials are published in the journal Frontiers in Immunology.
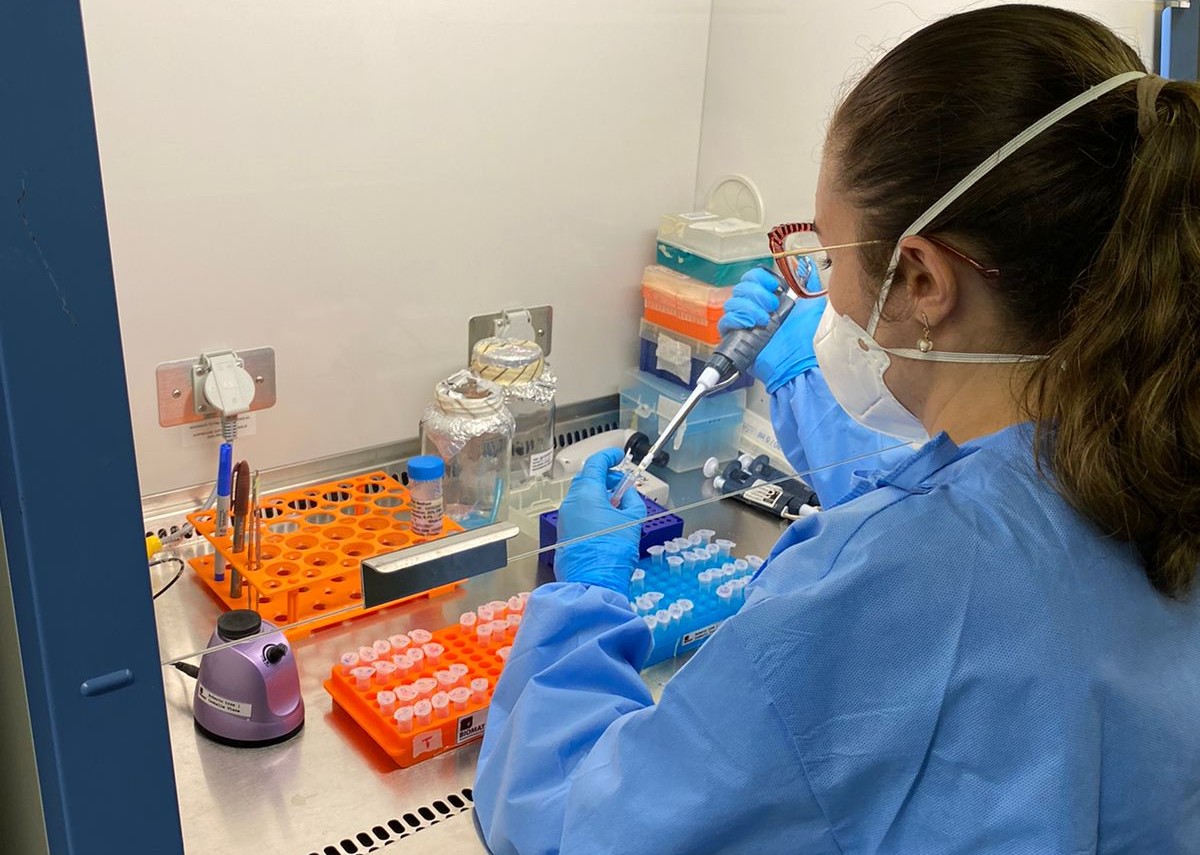
DNA vaccines are cheaper and potentially more efficient than inactivated or attenuated virus vaccines (scientist Francine Teixeira performing research at FM-USP; photo: Camilla Adan)
By Maria Fernanda Ziegler | Agência FAPESP – In Brazil, researchers at the University of São Paulo (USP) and the Pernambuco division of Oswaldo Cruz Foundation (FIOCRUZ) are developing a zika vaccine. The formulation was tested on mice and found to be efficacious, inducing an immune response against the virus and protecting the animals appropriately. The results are reported in an article published in the journal Frontiers in Immunology.
“Most vaccines use an attenuated or inactivated form of the virus they’re designed to combat. DNA vaccines are more advanced. The technology has evolved over the past 30 years to become a powerful therapeutic platform. In this study, we designed four DNA vaccine formulations encoding part of the viral envelope’s protein complex and selected the one that proved most efficacious,” said Maria Sato, a professor at the University of São Paulo’s Medical School (FM-USP) and corresponding author of the article.
In addition to being technologically more advanced, DNA vaccines tend to be cheaper and potentially more efficient than attenuated or inactivated virus vaccines. “It’s a low-cost technology and relatively easy to use because you can design a formulation by taking the key parts of the virus and adding [adjuvant] substances that boost the immune response. However, achieving sufficient immunogenicity [by triggering a robust immune response] is a challenge for DNA vaccines,” said Franciane Teixeira, first author of the article. The study it describes was part of her PhD research at FM-USP.
FAPESP supports the research group via two projects (19/25119-7 and 18/18230-6). Funding was also supplied by the Pernambuco State Science and Technology Foundation (FACEPE), the National Council for Scientific and Technological Development (CNPq), FIOCRUZ, and Horizon 2020 (European Union).
DNA vaccines
With the aid of molecular biology techniques, the researchers selected zika virus genes that encode two of its structural proteins – the pre-membrane/membrane (prM) protein and the envelope (E) protein – and deleted specific parts of the viral envelope. To keep the selected genetic sequences stable, they inserted each one into a plasmid. Plasmids are small circular DNA molecules obtained from bacteria that do not cause disease in humans and are widely used as vectors in genetic engineering.
When the vaccine is injected, the plasmid (the DNA vaccine proper) enters the host organism’s cell nuclei, where the encoded sequence is deciphered and proteins equal to zika’s are produced, leading the host’s defense cells to recognize them as viral particles, produce antibodies against the virus and trigger other protective mechanisms.
“It’s important to bear in mind that, like the messenger RNA vaccines produced by Pfizer and Moderna against SARS-CoV-2, DNA vaccines don’t alter the host organism’s genetic code, create a new species or cause autoimmune disease. The technology is safe, despite all the fake news and disinformation,” said Isabelle Viana, a researcher at FIOCRUZ Pernambuco and Teixeira’s co-supervisor.
“Humans are the result of billions of years of evolution and constant interaction with other DNAs, as happens when we’re infected by a pathogen, for example.”
Envelope protein
The target chosen by the researchers for the zika vaccine is the protein complex that comprises the outer surface of the virus, including the envelope protein, which is the primary trigger for the production of neutralizing antibodies. “We aimed at modulating the regions that make up the envelope protein, and to do so we removed the regions of this protein that bind it to the cell membrane, which are known as the stem and transmembrane portions,” Teixeira explained.
According to the authors of the article, the approach facilitated the enhanced expression of these zika proteins by the organism after immunization, leading to increased production of antibodies against the virus.
The formulation called ZK_ΔSTP, where the membrane-anchoring regions were completely removed, proved to be far more immunogenic than the other three designed by the research group. “This strategy corresponds to removal of the zika envelope protein cell membrane-anchoring region and promotion of extracellular protein expression. The vaccine induced a strong response by the adaptive immune system in adult mice, with high levels of neutralizing antibodies [in the humoral response] and production of T and B lymphocytes [in the cellular response],” Teixeira said.
The addition of aluminum hydroxide adjuvants led to a sustained neutralizing response, protecting the mice after they were exposed to the virus. “The results show that the formulation is efficacious and deserves to be developed further through more translational studies,” Teixeira said.
Challenges
Despite scientific progress since the last zika outbreak in the Americas, there are no approved vaccines or treatments for the disease. Besides economic issues, a peculiarity of the pathogen makes the development of a vaccine especially challenging: zika virus is very similar to all four serotypes of dengue virus.
“There’s a risk of what we call a cross-reaction, where antibodies produced by the zika vaccine recognize dengue virus. This may seem positive at first glance, but it can be a hazard without proper interpretation,” Viana said, adding that a second dengue infection is typically more severe than the first for several reasons.
“The patient will have produced antibodies against dengue in the first infection, and if they aren’t potent enough to prevent a second infection by a different dengue serotype, the opposite effect occurs: the antibodies bind to the virus and it penetrates cells more easily. In other words, the organism helps the virus infect its own cells.”
According to Viana, previous research by the group showed that practically the entire population of Brazil has immunity against at least one dengue serotype. “So in formulating a zika vaccine, it’s crucial to make sure this cross-reaction doesn’t occur in people who have had dengue. In our tests on mice, the vaccine we formulated induced neutralization only of zika, showing that it doesn’t recognize any dengue serotypes and doesn’t produce a cross-reaction,” he said.
The article “Enhanced immunogenicity and protective efficacy in mice following a Zika DNA vaccine designed by modulation of membrane-anchoring regions and its association to adjuvants” is at: www.frontiersin.org/articles/10.3389/fimmu.2024.1307546/full.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





