

A biodressing containing human umbilical cord stem cells was produced in a 3D printer by the startup In Situ Cell Therapy. Researchers at the University of São Paulo found that when used on diabetic mice, the “smart” biodressing modulated the immune response, stimulated collagen synthesis and enhanced tissue repair (image: In Situ Cell Therapy)
A biodressing containing human umbilical cord stem cells was produced in a 3D printer by the startup In Situ Cell Therapy. Researchers at the University of São Paulo found that when used on diabetic mice, the “smart” biodressing modulated the immune response, stimulated collagen synthesis and enhanced tissue repair.
A biodressing containing human umbilical cord stem cells was produced in a 3D printer by the startup In Situ Cell Therapy. Researchers at the University of São Paulo found that when used on diabetic mice, the “smart” biodressing modulated the immune response, stimulated collagen synthesis and enhanced tissue repair.
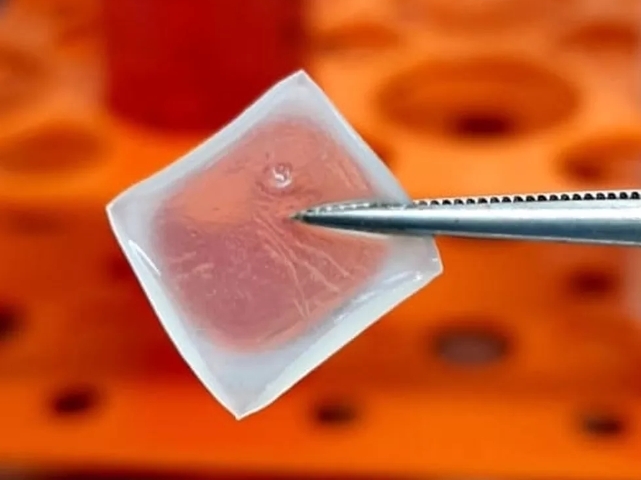
A biodressing containing human umbilical cord stem cells was produced in a 3D printer by the startup In Situ Cell Therapy. Researchers at the University of São Paulo found that when used on diabetic mice, the “smart” biodressing modulated the immune response, stimulated collagen synthesis and enhanced tissue repair (image: In Situ Cell Therapy)
By Thais Szego | Agência FAPESP – One of the most daunting challenges faced by people with type 1 diabetes is poor wound healing. This happens because an excessive amount of sugar in the bloodstream when the disease is not properly controlled hinders the shift from inflammation to tissue regeneration. To combat this complication of diabetes, a team at the University of São Paulo’s Ribeirão Preto Medical School (FMRP-USP) in Brazil tested a biodressing created by In Situ Cell Therapy, a startup based in the city’s Supera Innovation and Technology Park.
“It’s made with a substance called alginate hydrogel and contains human umbilical cord cells,” said Daniela Carlos Sartori, last author of the article on the study published in Regenerative Therapy. She led the research at FMRP-USP’s Metabolic Disease Immunoregulation Laboratory (LIDM).
The human umbilical cord mesenchymal stem cells (HUC-MSCs) used in the experiments are self-renewing and multipotent. They secrete numerous bioactive molecules with different functions in the healing process, including cytokines and growth factors responsible for immunomodulation, angiogenesis (creation of new blood vessels) and enhanced scar tissue quality.
“The production process involved 3D bioprinting with the support of a firm that specializes in additive manufacturing. It produced [the biodressing] precisely to match the size of the wound, with the correct distribution of mesenchymal cells in the hydrogel, which kept them viable during printing and use,” Sartori explained.
The 3D-printed biodressing is considered “smart” because it contains living cells capable of perceiving the signals emitted by the wound and responding by releasing cytokines and growth factor according to the tissue’s needs. As such, it is active in all stages of healing, whereas most conventional dressings merely cover the wound or treat it in a specific healing stage.
To validate its efficacy, the researchers induced type 1 diabetes in 18 mice. After 15 days, the animals were anesthetized, and the scientists made wounds by removing 1 square centimeter of skin from their backs, immediately dressing the wounds. The mice were divided into four groups: diabetic with biodressing not containing mesenchymal stem cells, diabetic with biodressing containing MSCs, non-diabetic with biodressing not containing MSCs, and non-diabetic with biodressing containing MSCs.
After ten days of treatment, the diabetic mice with biodressings that lacked MSCs displayed 50% wound closure, while the diabetic mice with “smart” biodressings that contained MSCs displayed 80% wound closure. This evidenced a significant improvement in healing when the biodressing with MSCs was used.
According to the article, the main reason was that MSCs administered by biodressings stimulate the immune system, which in turn has a direct impact on healing. Activated MSCs secrete several cytokines, including transforming growth factor-β (TGF-β). Expression of this growth factor increased in the diabetic mice that received the biodressing containing these cells, which are important to collagen synthesis and the repair of skin wounds.
The study was supported by FAPESP via two projects (18/14815-0 and 19/22013-3).
Clinical trials are required before the biodressing can be used to treat diabetic patients’ wounds. If the results are positive, approval of the product can be sought from ANVISA, Brazil’s national health surveillance agency.
The article “Xenogeneic mesenchymal stem cell biocurative improves skin wounds healing in diabetic mice by increasing mast cells and the regenerative profile” is at: www.sciencedirect.com/science/article/pii/S2352320422001286?via%3Dihub.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





