

The graph (A) shows the conformational change to the SARS-CoV-2 spike protein in the presence of heparin. In the image of the spike protein (B), the dark blue regions represent the potential heparin binding sites (image: INFAR-UNESP)
Laboratory tests conducted by collaborating Brazilian and European researchers showed that heparin alters the shape of the protein used by SARS-CoV-2 to penetrate host cells.
Laboratory tests conducted by collaborating Brazilian and European researchers showed that heparin alters the shape of the protein used by SARS-CoV-2 to penetrate host cells.
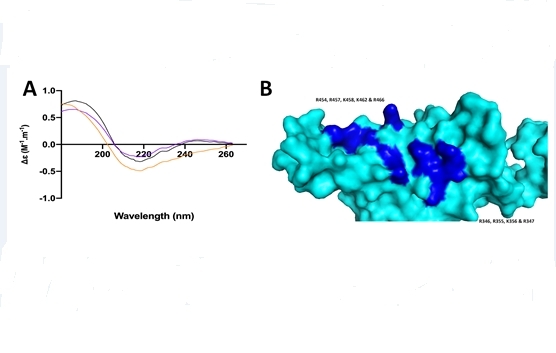
The graph (A) shows the conformational change to the SARS-CoV-2 spike protein in the presence of heparin. In the image of the spike protein (B), the dark blue regions represent the potential heparin binding sites (image: INFAR-UNESP)
By Elton Alisson | Agência FAPESP – A study conducted by Brazilian researchers affiliated with the Federal University of São Paulo (UNIFESP) and European collaborators has revealed a possible novel mechanism of the drug heparin in the treatment of COVID-19. In addition to combating coagulation disorders that affect lung vessels and impair oxygenation, heparin also appears to hinder cell penetration by the coronavirus SARS-CoV-2.
In laboratory tests using Vero cells, administration of heparin led to a 70% reduction in cell invasion by this virus.
Vero cells are a lineage derived from the kidneys of African green monkeys (Chlorocebus sp., formerly called Cercopithecus aethiops), and are commonly used in microbiology and molecular research.
The study was supported by FAPESP via a project selected in its recent call for proposals entitled “Fast-track supplements for projects against COVID-19”.
The findings are described in an article published on the platform bioRxiv, in a preprint (not yet peer-reviewed) version. Scientists in the UK and Italy also participated.
“There were already indications that heparin, a drug that performs various pharmacological functions, could also prevent infection by coronaviruses and other viruses but the evidence was not very robust. We succeeded in proving this property of the drug experimentally in vitro,” Helena Bonciani Nader, a professor at UNIFESP, told Agência FAPESP. Nader was principal investigator for the project on the Brazilian side.
Nader’s group have studied glycosaminoglycans (the class of complex carbohydrates to which heparin belongs) for more than 40 years, and developed the first low molecular weight heparins, used clinically to prevent blood clots and treat thrombosis, including in COVID-19 patients.
Among the group’s achievements during this period is the discovery that heparin is a multi-target drug: besides its blood-thinning properties it can bind to various proteins, including growth factors and cytokines that attach to specific target cell surface receptors.
Studies conducted by other groups in recent years suggest that surface proteins in other coronaviruses can also bind to the closely related glycosaminoglycan heparan sulphate in order to infect mammalian cells.
With the emergence of SARS-CoV-2, the UNIFESP researchers and collaborators in the UK and Italy had the idea of investigating whether its spike protein – the surface protein it uses to invade human cells – would bind to heparin, as the drug has a similar molecular structure to that of heparan sulfate.
The experiments validated the hypothesis. Surface plasmon resonance and circular dichroism spectroscopy were used to confirm that heparin indeed binds to the spike protein of SARS-CoV-2, changing its molecular conformation and preventing it from invading human cells.
“If it can’t invade cells, it can’t multiply and the infection fails,” Nader said.
Best structure
The researchers also analyzed the various possible structures that best enabled heparins to interact with the virus and change the conformation of its spike protein. To this end they used a library of heparin derivatives and size-defined fragments of the molecule.
“The results of the analysis showed that heparin interaction is most effective in inducing a conformational change in the spike protein of SARS-CoV-2 with six polysaccharides, that is, a hexasaccharide,” Nader said.
The researchers are now experimenting with structural changes to heparins with the aim of identifying a molecule that has the same efficacy in terms of binding to the virus and altering the conformation of its spike protein but causes less bleeding, a potential side-effect of the drug.
They are also testing other compounds called heparin mimetics because they mimic the action of heparin proper. “Our goal is to select the molecule with the best anti-viral effect,” said Nader, who is also a member of FAPESP’s Board of Trustees.
The ongoing studies, she explained, use different cellular models and structural biology techniques such as nuclear magnetic resonance, stopped-flow kinetics of fast reactions, confocal microscopy and flow cytometry, among others.
The article “Heparin inhibits cellular invasion by SARS-CoV-2: structural dependence of the interaction of the surface protein (spike) S1 receptor binding domain with heparin” (doi: 10.1101/2020.04.28.066761) by Courtney J. Mycroft-West, Dunhao Su, Isabel Pagani, Timothy R. Rudd, Stefano Elli, Scott E. Guimond, Gavin Miller, Maria C. Z. Meneghetti, Helena B. Nader, Yong Li, Quentin M. Nunes, Patricia Procter, Nicasio Mancini, Massimo Clementi, Nicholas R. Forsyth, Jeremy E. Turnbull, Marco Guerrini, David G. Fernig, Elisa Vicenzi, Edwin A. Yates, Marcelo A. Lima and Mark A. Skidmore can be read on bioRxiv at: www.biorxiv.org/content/10.1101/2020.04.28.066761v1.full.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





