

Electron micrograph image of spermatozoon from a COVID-19 patient (photo: Jorge Hallak et al./Andrology)
Researchers detected SARS-CoV-2 in male reproductive cells under the microscope even when PCR testing failed to detect the virus in semen. The discovery serves as a warning of possible implications for natural conception and particularly for assisted reproduction.
Researchers detected SARS-CoV-2 in male reproductive cells under the microscope even when PCR testing failed to detect the virus in semen. The discovery serves as a warning of possible implications for natural conception and particularly for assisted reproduction.
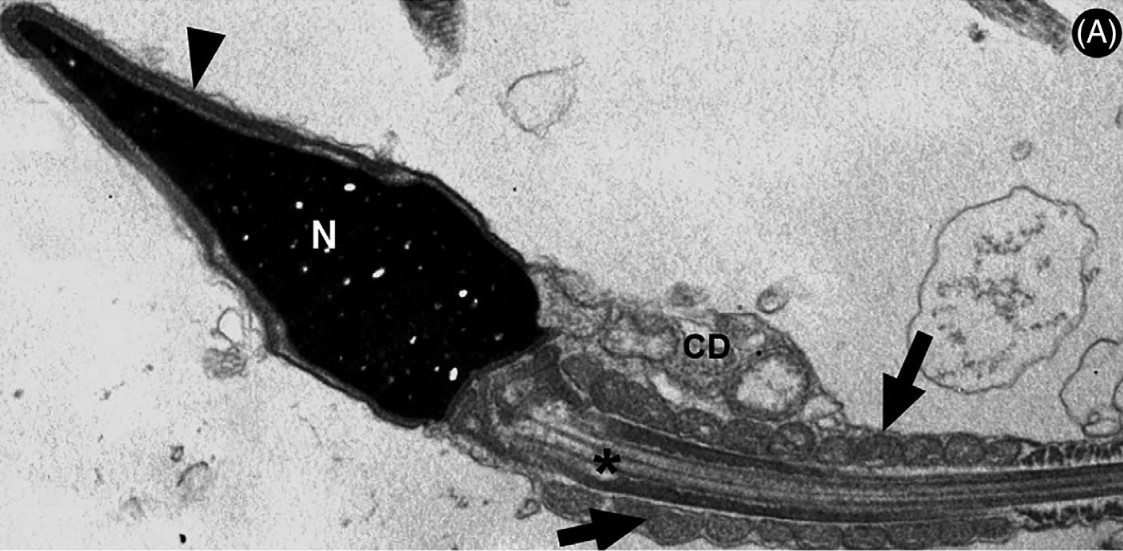
Electron micrograph image of spermatozoon from a COVID-19 patient (photo: Jorge Hallak et al./Andrology)
By Julia Moióli | Agência FAPESP – Researchers at the University of São Paulo (USP) in Brazil have shown for the first time that SARS-CoV-2, the virus that causes COVID-19, can remain in the sperm of patients for up to 90 days after hospital discharge and up to 110 days after the initial infection, reducing semen quality. The study is reported in an article published in the journal Andrology. The authors suggest that people who plan to have children should observe a period of “quarantine” after recovering from COVID-19.
More than four years after the start of the pandemic, we know SARS-CoV-2 is able to invade and destroy several types of human cells and tissue, including the reproductive system, where the testicles serve as a “gateway”. Although scientists have noted that the virus is more aggressive than other viruses toward the male genital tract, and autopsies have found it in testicles, it has rarely been detected in semen by polymerase chain reaction (PCR) analysis, which focuses on viral DNA.
To fill this knowledge gap, the study – which was supported by FAPESP – used real-time PCR and transmission electronic microscopy (TEM) to detect viral RNA in semen and spermatozoa donated by men who were convalescing from COVID-19.
The semen samples were taken from 13 patients aged between 21 and 50 who had had mild, moderate and severe COVID-19 and had been admitted to Hospital das Clínicas (HC), the hospital complex run by the university’s medical school (FM-USP). The analysis was conducted up to 90 days after discharge and 110 days after diagnosis. Although the PCR test results were negative for SARS-CoV-2 in semen in all cases, the virus was detected in sperm from eight of 11 moderate to severe COVID-19 patients (72.7%) within 90 days of discharge, which does not mean it was not present for longer, according to the authors.
SARS-CoV-2 was also detected in one of the mild COVID-19 patients. In sum, the virus was detected in sperm from nine of the 13 patients (69.2%). Two others had ultrastructural gamete impairment similar to that seen in patients with a COVID-19 diagnosis. The authors therefore concluded that 11 of the patients had the virus in their sperm.
“Moreover, we found that the sperm produced ‘extracellular traps’ based on nuclear DNA. In other words, genetic material in the nucleus decondensed, the sperms’ cell membranes ruptured, and the DNA was expelled into the extracellular medium, forming networks similar to those described previously in the systemic inflammatory response to SARS-CoV-2,” said Jorge Hallak, a professor at FM-USP and corresponding author of the article.
The networks in question are neutrophil extracellular traps (NETs). Neutrophils, a type of white blood cell, form the first line of the immune system, immobilizing and killing pathogenic bacteria, fungi and viruses. When hyperactive, however, NETs can harm tissue elsewhere in the organism (read more at: agencia.fapesp.br/33523).
TEM analysis showed that the sperm produced extracellular traps based on nuclear DNA to neutralize the pathogen, “sacrificing themselves” to contain the pathogen in a mechanism known as a suicidal ETosis-like response (ETosis meaning death via extracellular traps).
“The finding that spermatozoa are part of the innate immune system and help defend the organism against attack by pathogens is unique in the literature and makes the study very important. It can be considered a scientific paradigm shift,” Hallak said.
Until now, he added, sperm were known to have four functions: binding the genetic contents of male gametes to female gametes, fertilizing female gametes, promoting embryo development until the twelfth week of pregnancy, and co-determining the development of certain chronic diseases in adulthood, such as infertility, hypogonadism, diabetes, hypertension, some types of cancer, and cardiovascular disorders, among others.
The discovery described in the study adds a novel function to their role in reproduction. “The possible implications of our findings for the use of sperm in assisted reproduction should be urgently considered by physicians and regulators, especially with regard to the technique used by Brazilian laboratories that perform gamete micromanipulation in more than 90% of cases of conjugal infertility, which involves the injection of a single spermatozoon into the egg and is known as intracytoplasmic sperm injection, or ICSI,” Hallak said.
Hallak advocates postponement of natural conception and particularly of assisted reproduction for at least six months after infection by SARS-CoV-2, even if mild COVID-19 ensues.
Previous discoveries
Hallak was one of the first members of the scientific and medical communities to suggest more caution in reproduction protocols during the pandemic. He has studied the impact of COVID-19 on reproductive and sexual health since 2020, when he volunteered on the front line as an emergency room physician at HC-FM-USP.
His research group, which includes colleagues in FM-USP’s Department of Pathology, has already made important discoveries in the field, such as the higher risk of severe COVID-19 infection and death from the disease for men simply because of their sex, possibly because of the abundance of ACE2 receptors and TMPRSS2 in testes, whereas ovaries have only ACE2 receptors. The virus uses ACE2 to invade cells; TMPRSS2 is a protein that enables the virus to bind to ACE2 on the cell surface.
In a study conducted with members of HC-FM-USP’s Clinical Urology Division, the group found that health workers experienced a sharp drop in libido and sexual satisfaction, as well as increased consumption of pornography and more frequent masturbation, due to the pandemic.
The group also discovered that the testes are potential targets for infection by the virus, which causes subclinical epididymitis (inflammation of the epididymis, a narrow tube attached to each testicle that stores, matures and transports sperm cells), and showed for the first time the severity of the testicular lesions associated with COVID-19.
The group of physicians and scientists at HC-FM-USP, led by Professor Carlos Carvalho, is currently investigating the lagging effects of infection by SARS-CoV-2 in more than 700 patients originally assessed for a Thematic Project funded by FAPESP.
The article “Transmission electron microscopy reveals the presence of SARS-CoV-2 in human spermatozoa associated with an ETosis-like response” is at: onlinelibrary.wiley.com/doi/abs/10.1111/andr.13612.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





