

Image: Demedia
A startup supported by FAPESP is developing an app that leverages artificial intelligence to help users monitor the disease and improve the quality of their lives.
A startup supported by FAPESP is developing an app that leverages artificial intelligence to help users monitor the disease and improve the quality of their lives.
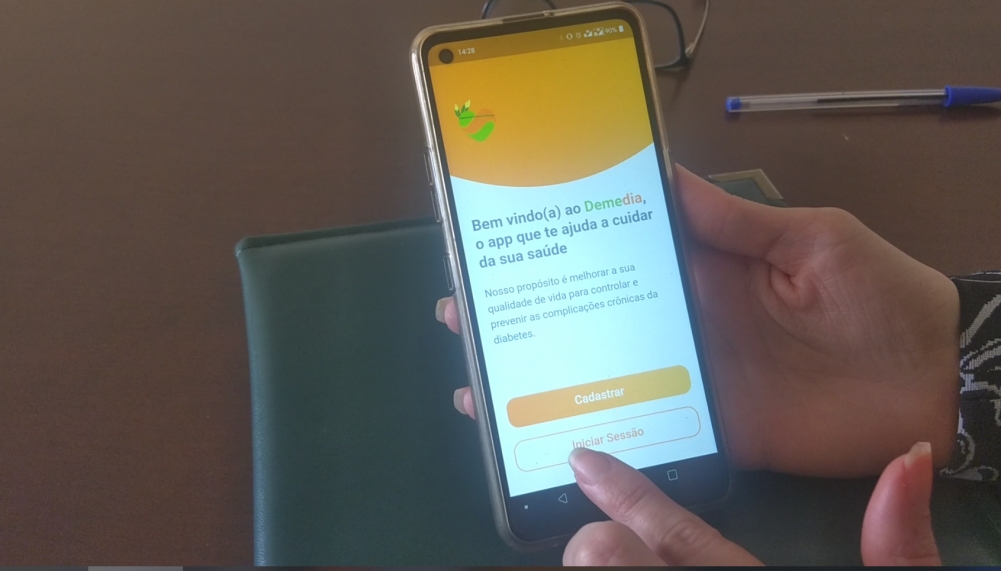
Image: Demedia
By Rodrigo de Oliveira Andrade | FAPESP Innovative R&D – A new digital platform promises to help users control and prevent chronic complications of diabetes, a disease in which the organism cannot efficiently metabolize sugar (glucose) in the blood.
Users of the related smartphone app receive personalized medical advice from Demedia, a tool based on information and communication technology (ICT) and artificial intelligence (AI), so that they can monitor the disease, prevent it from becoming more severe, and control key aspects of their own healthcare to improve the quality of their lives.
The platform was established in 2021 as a collaboration between Demed Tecnologia em Saúde, a startup headquartered in São Paulo city, Brazil, and the innovation program (Inova) run by the Armed Forces Hospital in Brasilia (HFAB).
Demedia is currently supported by FINEP, the Brazilian Innovation Agency, via the Centelha (“Spark”) program, a federal government initiative to foster innovative ventures nationwide. In São Paulo state, Centelha is co-funded by FAPESP.
The platform is now being validated technologically and for scalability in a project involving more than 100 patients at HFAB and in Indigenous communities in the states of Ceará and Maranhão.
Control and automation engineer Marcia Ferraresi de Araújo, a founding partner of the startup and director of the platform, explained that patients diagnosed with diabetes are introduced to the platform by physicians and nurses in the hospitals that are participating in the validation exercise. The patients are then invited to download the app to their smartphones. “In the case of Indigenous patients, use of the app is intermediated by nurses and Indigenous health workers in the community,” she said.
Once users have registered and entered their details into the app, they can watch videos featuring an endocrinologist and other health professionals elucidating the mechanisms of the disease and its prevention and control.
The platform also offers a chatbot based on AI software, which creates realistic texts in response to questions and prompts, simulating conversation with a person. The aim is for users interact with the chatbot to find out more about diabetes. According to Araújo, it has been trained on medical information and recommendations to make sure its answers are reliable.
Patient interaction with the AI fuels a gamification platform (inspired by online computer games) to create a dynamic that supports patient education on diabetes and self-care in accordance with their health profile, in a strategy designed to assure adherence to the treatment.
A predictive model based on the user’s health profile and past use of the app sets goals. “Our system records terms and keywords as chatbot interaction takes place. This data is used later to model the gamification goals,” Araújo said, citing as an example the case of a patient who interacted with the chatbot on the subject of preventing the indisposition and lightheadedness or blackouts caused by hypoglycemia due to insulin spikes resulting in a sharp drop in blood sugar. “Data from interaction with the chatbot is fed into the gamified platform, leading it to suggest goals based on medical guidelines to help prevent hypoglycemia.”
The platform sends alerts to remind users to take medication. Goals can also be dietary and exercise-related, always in connection with the user’s health status. Every goal met earns a reward in the shape of a digital “coin” that can be converted into a discount on purchases of goods or services relating to control of diabetes, such as low-sugar foods, devices for measuring blood pressure, lancets, glucometers, and Pilates classes, among others.
“Many patients can’t afford these foods and devices, and they may reduce or abandon the treatment prescribed by their physician or healthcare team as a result,” Araújo said.
Goal validation is manual: patients themselves use the app to record whether goals are met or missed. Reports on treatment history can be generated from app usage dynamics data. “The reports can be shared with physicians, provided patients give permission. Of course, we comply with the legislation on privacy and personal data protection. Healthcare professionals can use all this information to obtain a more detailed picture of each patient’s condition,” she explained.
The data can also be anonymized and used to produce broader epidemiological reports that support the work of healthcare professionals and institutions in planning preventive measures for diabetics, especially in primary and secondary care. “This strategy has the potential to reduce the risk of chronic complications associated with diabetes and the economic impact on the health service, such as the cost of preventable procedures and hospitalizations,” she said.
Next steps will include refining the platform and evaluating outcomes for patients who use it. “We want to know how much Demedia helps control clinical indicators such as glycated hemoglobin [which measures blood glucose control over a period of two to three months], and metabolic syndrome indicators such as cholesterol, blood pressure and visceral fat, as well as microalbuminuria, creatinine and retinopathy,” she said. “We want to know how far our strategy can help control and prevent complications induced by diabetes.”
The startup hopes to be able to extend the platform’s scope so that it can help prevent or control other non-transmissible chronic diseases, such as cardiovascular and respiratory disorders, as well as some types of tumor. It also plans to widen access to Demedia for more Indigenous communities.
Brazil has about 15 million diabetics, ranking fifth in the world in terms of countrywide incidence of the disease. The number could reach 21.5 million by 2030, according to projections by the International Diabetes Federation (IDF).
Most have type 2 diabetes, where the body either does not produce enough insulin or resists insulin. Many are unaware they have the disease. Others are unable to control their blood sugar and abandon treatment, which is complex and hard to maintain.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





