

A formulation used in preclinical trials was produced at the Butantan Institute’s Special Vaccine Development Laboratory (images: bioreactors for bench-scale production (A); bioreactor for pilot-scale production (B) / Butantan Institute)
A formulation developed in Brazil is expected to protect against all 90-odd serotypes of the Streptococcus pneumoniae bacterium. Vaccines currently available in Brazil are effective against 13 serotypes at most.
A formulation developed in Brazil is expected to protect against all 90-odd serotypes of the Streptococcus pneumoniae bacterium. Vaccines currently available in Brazil are effective against 13 serotypes at most.
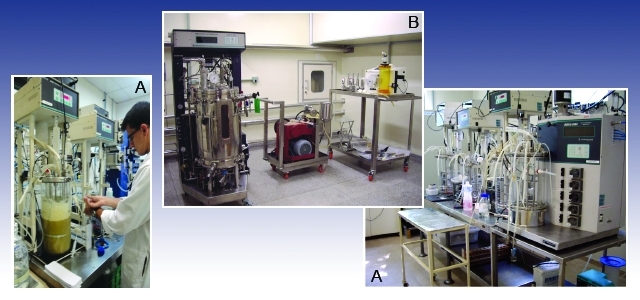
A formulation used in preclinical trials was produced at the Butantan Institute’s Special Vaccine Development Laboratory (images: bioreactors for bench-scale production (A); bioreactor for pilot-scale production (B) / Butantan Institute)
By Maria Fernanda Ziegler | Agência FAPESP – A novel vaccine against pneumonia that is less expensive and more effective than those currently used in Brazil is being tested in human patients. Developed by researchers at the Butantan Institute (Brazil) and Boston Children’s Hospital, part of the Harvard Medical School (USA), the innovation is capable of providing protection against all serotypes of the bacterium Streptococcus pneumoniae.
“We chose a different strategy to activate the immune response. Instead of targeting the polysaccharides present in the bacterial capsule, as currently available vaccines do, we opted for proteins common to all serotypes of the microorganism,” said Luciana Cezar de Cerqueira Leite, a researcher in the Butantan Institute’s Special Vaccine Development Laboratory.
The initial research was led by Cerqueira Leite and supported by FAPESP. Phase I and II clinical trials were conducted in Africa and coordinated in the US by the Harvard team, with support from the Bill & Melinda Gates Foundation and the Program for Appropriate Technologies in Health (PATH), a Seattle-based nonprofit dedicated to developing innovations that save lives and improve health.
“It took more than ten years of research to arrive at this cellular vaccine,” Cerqueira Leite said. “First, we investigated proteins that could be used as targets. The idea of developing a cellular vaccine occurred to us on the way. We designed the production process and changed the adjuvant [an agent used in conjunction with the vaccine antigen to augment the host’s immune response] as well as the administration pathway. Initially, we set out to produce an intranasally administered vaccine, but then we realized that the product would be more efficient if it was administered by intramuscular injection.”
Polyvalent
Some 90 serotypes of S. pneumoniae are estimated to exist worldwide. In addition to pneumonia, the bacterium causes meningitis, otitis and sinusitis, among other diseases. The serotypes are defined on the basis of the combination of polysaccharides present in the microorganisms’ capsule. In conventional vaccines, this combination determines the antigen to be introduced into the organism to stimulate antibody production. The vaccine developed by the Butantan Institute triggers an immune response regardless of the bacterial serotype.
“We cultured the bacterium without its capsule in the lab and used a special technique to kill it without disintegrating it. So, the inactivated bacterium can be administered as a vaccine. We also identified immunogenic proteins that are common to all S. pneumoniae serotypes,” Cerqueira Leite said.
In a recent article published in the journal Expert Review of Vaccines, Cerqueira Leite and collaborators stressed the importance of developing an affordable pneumonia vaccine that is effective against all S. pneumoniae serotypes.
“In the specific case of pneumonia, insisting on the inclusion of new serotypes in conjugate vaccines only leads to increased complexity and higher production costs, making already expensive vaccines even less affordable for developing countries like Brazil,” Cerqueira Leite said.
The pneumococcal vaccines currently available are effective against between ten and 13 serotypes, she added. A nonconjugate version covers 23 serotypes but is used mainly to immunize adults, as it is not effective in children.
“The first generation of conjugate vaccines was effective against the seven most prevalent serotypes in Europe and the US [7-valent]. However, because prevalence varied from one region to another, in Brazil it wasn’t able to provide very good coverage, only about 60%,” she said.
As time passed, it became possible to combine more strains, and eventually 10-valent and 13-valent vaccines were produced, “but there’s a problem with this strategy,” Cerqueira Leite said. “When you take specific serotypes out of circulation, other strains [with different serotypes] emerge naturally, and the existing vaccines lose their efficacy. This is known as serotype substitution.”
As well as being more comprehensive than current vaccines, the cellular vaccine developed by the Butantan Institute is not vulnerable to the problem of serotype substitution. Pricing is another advantage, according to Cerqueira Leite. “It’s hard to say exactly how much the vaccine will cost before it’s even been approved and produced, but we estimate about two dollars. The polysaccharide vaccine [13-valent] currently costs the citizen who uses a private clinic about 60 dollars. Public services [administered under the umbrella of SUS, Brazil’s national health system] pay 15 dollars,” she said.
The price is lower largely because the production process is less complex. “To make the 13-valent vaccine, each of the 13 different serotypes has to be cultured separately and purified to obtain the polysaccharides. Also, because it’s a conjugate vaccine, a reaction has to be produced between the polysaccharide and a carrier protein. There are several stages. It’s a laborious process with several stages and takes almost two years,” she said.
The new vaccine can be produced in approximately two months, according to Cerqueira Leite.
Phase I and II clinical trials have been completed, analyzing safety and toxicity and validating immunogenicity, respectively. “We plan to hold another phase II trial in the US. This is the stage where you compare the type of immune response produced in the populations of different countries,” she said.
Phase III clinical trials involve a larger number of people and test the vaccine’s effectiveness by comparing an immunized group with a group that receives a placebo. A phase III trial has yet to be scheduled for the new vaccine.
The article “The long search for a serotype independent pneumococcal vaccine” (doi: 10.1080/14760584.2020.1711055) by T.R. Converso, L. Assoni, G.O. Andréa, M. Darrieux and L.C.C. Leite can be retrieved from www.tandfonline.com/doi/full/10.1080/14760584.2020.1711055.
Republish
The Agency FAPESP licenses news via Creative Commons (CC-BY-NC-ND) so that they can be republished free of charge and in a simple way by other digital or printed vehicles. Agência FAPESP must be credited as the source of the content being republished and the name of the reporter (if any) must be attributed. Using the HMTL button below allows compliance with these rules, detailed in Digital Republishing Policy FAPESP.





